The fentanyl crisis is reshaping lives across Canada, leaving families searching for answers and individuals desperate for change. Recovery begins with understanding the landscape of treatment—a path that’s as varied as the people it’s meant to help.
Whether through intensive medical care, community-driven support, or life-saving medications, Canada’s resources offer hope for turning the tide.
Let’s chart the options, debunk the complexities, and explore the road to recovery.

Treatment That Works: Breaking Free from Fentanyl
From full-time care to flexible programs, treatment isn’t one-size-fits-all. Here’s how different options stack up:
1. The 24/7 Shield: Inpatient Rehabilitation
Sometimes, recovery means stepping away from the chaos of daily life. Inpatient rehab provides round-the-clock medical care and a safe, controlled environment to heal.
- Why It’s Effective: Offers immediate medical attention for withdrawal symptoms and a structured path to recovery.
- Canadian Examples: Public programs like OHIP-supported centers and private facilities catering to specialized care.
Pacific Interventions in Vancouver, British Columbia, offers comprehensive inpatient rehabilitation services tailored to individuals battling fentanyl addiction.
Our client-centered approach combines evidence-based treatment methods with personalized care plans to address each individual’s unique needs.
Services include medical detoxification, one-on-one counseling, group therapy, and aftercare planning, all within a supportive and structured environment.
2. Life Meets Recovery: Outpatient Therapy
For those balancing work, family, or other commitments, outpatient programs deliver care without uprooting daily life.
- Why It’s Effective: Flexibility paired with expert counseling and medication management.
- Cost Considerations: Public health plans often cover basic services, but private care costs can vary.
3. Science on Your Side: Medication-Assisted Treatment (MAT)
Fentanyl doesn’t just grip the mind—it takes hold of the body. Medications like methadone and buprenorphine tackle physical dependence, giving people a fighting chance.
- Why It’s Effective: Helps manage cravings and stabilize lives for those committed to recovery.
- Quick Stat: Studies show MAT reduces overdose deaths by over 50%.
Life-Saving Medications: What You Need to Know!
Medications play a critical role in fentanyl addiction recovery, offering relief from withdrawal and reducing cravings. They provide stability and a vital pathway to long-term healing.
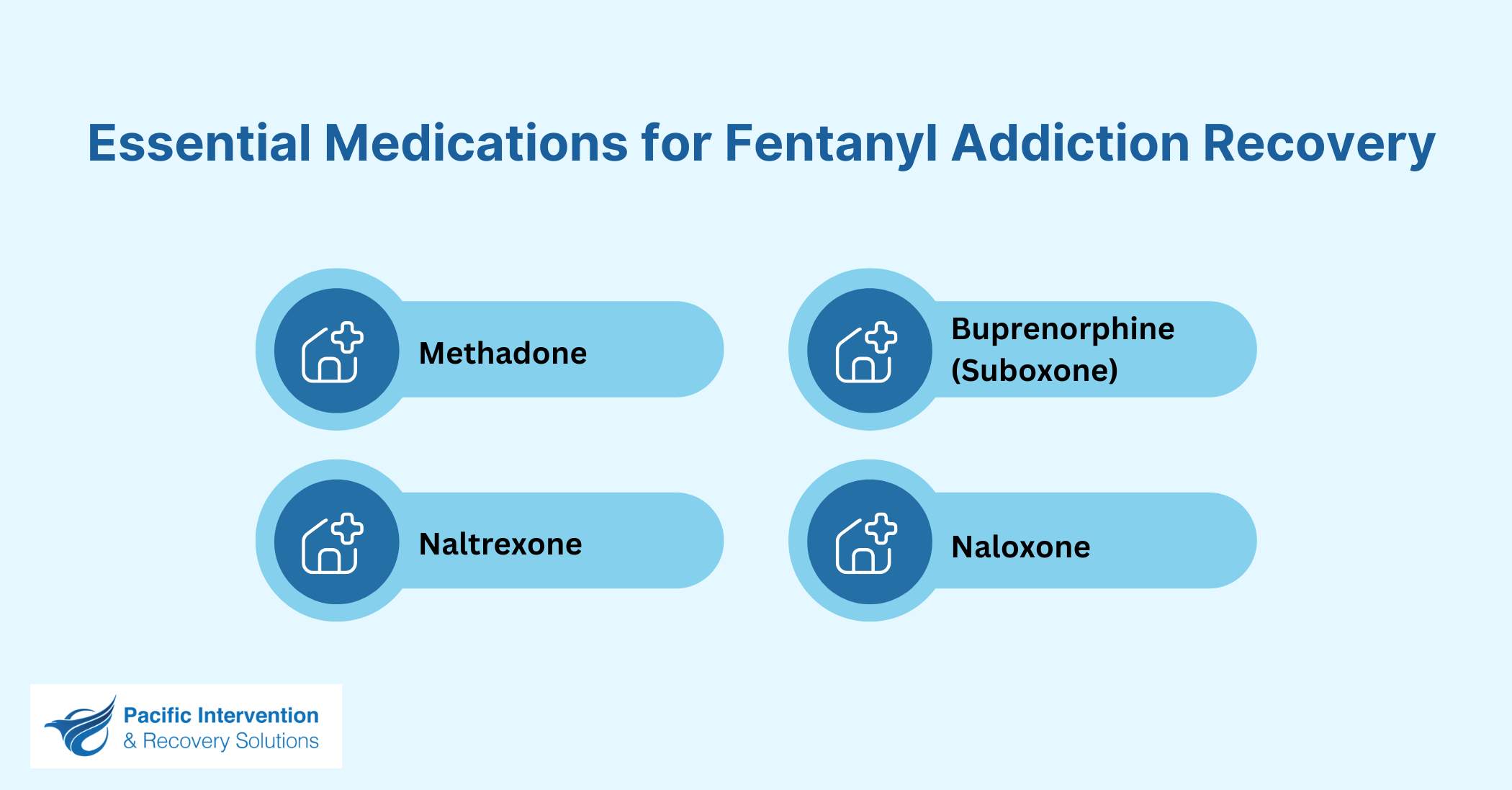
Methadone: A Steady Hand in the Storm
Methadone is a long-acting opioid agonist that reduces cravings and withdrawal symptoms. It binds to the same receptors as fentanyl but doesn’t produce the same intense high. Public clinics across Canada offer methadone through Opioid Agonist Therapy (OAT). Its ability to lower overdose risks makes it a key part of many recovery programs.
Buprenorphine (Suboxone): A Balanced Approach
Buprenorphine, or Suboxone, is a partial opioid agonist. It eases cravings and blocks the effects of other opioids, lowering the chances of relapse. Many individuals prefer Suboxone for outpatient recovery due to its flexibility. It’s also widely covered by provincial health plans, making it accessible to those in need.
Naltrexone: A Potent Blocker
Naltrexone works differently from other medications. It blocks opioids entirely, preventing any euphoric effects. This option is best for those who have already detoxed and are committed to sobriety. Available as a daily pill or monthly injection, it’s a powerful tool to reduce relapse for those ready to take the next step.
Naloxone: A Lifeline in Overdose Situations
Naloxone isn’t a treatment for addiction but a critical emergency tool. This opioid antagonist reverses overdoses by displacing fentanyl from brain receptors, restoring breathing. Widely available through Canadian pharmacies and harm reduction programs, free kits ensure timely, life-saving intervention.
Note: Medications are not a cure-all, but they form a strong foundation when paired with counseling and community support. Tailored to individual needs, these tools bring hope and stability to the recovery journey.
How long does fentanyl addiction treatment take?
The duration of treatment for fentanyl addiction varies based on individual needs and the severity of the addiction.
Detoxification, the first phase, typically lasts 5-10 days as the body clears fentanyl.
Medication-assisted treatments, such as methadone or Suboxone, may continue for months or even years, depending on the patient’s progress.
Inpatient rehabilitation programs often last 30-90 days, offering intensive care and therapy.
Outpatient programs are more flexible and can extend for several months.
Recovery is an ongoing process, with long-term support like counseling or community groups playing a critical role in maintaining sobriety and preventing relapse.
Community Support: Finding Strength Together
Recovery takes a village. Community-driven resources create safety nets for individuals and families grappling with fentanyl addiction:
- Support Groups That Stick: Programs like Narcotics Anonymous or SMART Recovery bring shared stories and accountability to the table.
- Harm Reduction, Life Extension: Supervised consumption sites and naloxone distribution save lives, one intervention at a time.
- Provincial Help Lines: Alberta’s 24/7 helpline (1-866-332-2322) and BC’s crisis line (1-800-SUICIDE) connect people with immediate resources.
Turning the Corner: Finding Your Way Out
Choosing a treatment plan means asking the tough questions:
- How severe is the addiction?
- What financial and local resources are available?
- Can I commit to a structured or flexible program?
Canada’s healthcare system, supported by organizations like Pacific Interventions, ensures you don’t have to face these questions alone.
Are there free addiction treatment options in Canada?
Yes, Canada offers several free or low-cost options through provincial healthcare systems.
Services like detox programs, outpatient counseling, and medication-assisted treatment are often covered by health insurance plans, such as OHIP in Ontario or BC Recovery Services.
Harm reduction initiatives, including naloxone kits and supervised consumption sites, are also freely available in many areas.
For inpatient rehabilitation, public facilities may have waiting lists, while private centers often require out-of-pocket payments.
Reaching out to provincial helplines or local healthcare providers is a good starting point to explore these accessible options.
Conclusion: Your Recovery Journey Starts Here
Fentanyl addiction is challenging, but recovery is possible. Canada offers diverse treatment options, including rehab, medications, and harm reduction programs. Paired with community support, these resources provide a strong foundation for reclaiming a healthy, fulfilling life.
Recovery is unique for everyone. Exploring resources like personalized care plans and provincial programs helps individuals find the best treatment. With compassion and evidence-based support, success is possible.
If you or someone you know is struggling with fentanyl addiction, Pacific Interventions is here to help. With expertise, empathy, and tailored solutions, they provide the guidance needed to navigate this challenging journey. Reach out today and take the first step toward healing.



