Substance use and mental health are deeply interconnected. Many people turn to drugs or alcohol as a way to cope with stress, anxiety, or depression, but this often leads to addiction and worsened mental health outcomes.
In other cases, existing mental health conditions are aggravated by substance use, creating what is known as dual diagnosis. Understanding how different substances impact mental health—both negatively and positively—is crucial for individuals and families seeking help.
While some substances can intensify mental health challenges, others are being researched and used in medical treatments for conditions like depression and PTSD. This guide examines the complex relationship between substance use and mental health, highlighting drugs that cause harm, those that offer potential therapeutic benefits, and pathways to recovery.
At Pacific Interventions, we are dedicated to helping individuals struggling with addiction and mental health issues. Our evidence-based treatment strategies empower individuals to regain control of their lives and achieve lasting recovery.
Understanding Substance-Related Mental Health Disorders
Substance-related mental health disorders occur when drugs or alcohol directly cause or worsen mental health conditions. These disorders often arise from the substances’ effects on the brain, leading to chemical imbalances that disrupt normal functioning.
In some cases, lifestyle factors associated with addiction—such as isolation, financial difficulties, or strained relationships—contribute to mental health challenges. For example, excessive alcohol use can lead to depression, while stimulants like cocaine and methamphetamine may heighten anxiety or paranoia.
Certain substances, such as cannabis or hallucinogens, can trigger psychotic symptoms or hallucinations, particularly in individuals predisposed to mental health issues. Understanding these risks is crucial for addressing the link between substance use and mental health disorders effectively.

What is dual diagnosis?
Dual diagnosis, or co-occurring disorders, refers to the simultaneous presence of a substance use disorder (SUD) and a mental health disorder. This condition is more common than many realize, with studies showing that around 50% of individuals with SUDs also have a mental health disorder.
Mental health conditions and SUDs are often interconnected. For instance, some individuals with alcohol addiction may also experience depression or anxiety. Others might turn to stimulants like methamphetamine to cope with untreated conditions such as ADHD or PTSD.
Dual diagnosis is especially prevalent among teenagers, individuals with serious mental illnesses, and those with specific mental health disorders. These overlapping issues often exacerbate one another, creating a complex situation that requires specialized, integrated care for effective treatment.
Why is identifying dual diagnosis crucial?
Accurately identifying dual diagnosis is essential because treating only one aspect—addiction or mental health—can result in incomplete recovery or relapse. For instance, if someone struggling with depression and alcoholism receives treatment solely for addiction, the untreated depression may trigger a relapse. Similarly, addressing depression without managing substance use can hinder mental health treatment and prolong recovery.
Dual diagnosis requires an integrated approach that addresses both addiction and mental health issues simultaneously. This holistic focus ensures lasting recovery and promotes overall mental well-being by treating the whole person rather than isolated symptoms.
Why do substance use disorders and mental disorders occur together?
While substance use disorders (SUDs) and mental health disorders often occur together, one does not necessarily cause the other. Researchers have identified three main reasons these conditions frequently coexist:
- Shared Risk Factors: Genetics, stress, and childhood trauma can increase the likelihood of both SUDs and mental health disorders. For example, veterans with PTSD are at a higher risk for developing SUDs.
- Self-Medication: People with mental disorders may use drugs or alcohol to temporarily relieve symptoms, a behavior known as self-medication. This can alter the brain and increase vulnerability to addiction.
- Substance-Induced Mental Disorders: Prolonged substance use can change brain chemistry, making individuals more susceptible to developing mental health disorders.
Understanding these connections is crucial for effective prevention and treatment of co-occurring conditions.

What drugs cause mental health issues?
Drug-induced mental illness is a serious concern that can worsen over time without treatment. While the initial effects of drugs or alcohol may seem appealing, they can cause significant harm to both the body and mind.
The risk of mental health issues is highest with long-term or heavy use, but even short-term or occasional use can lead to problems. The following list highlights substances commonly associated with specific mental health disorders. While not exhaustive, it underscores the severe risks of untreated drug and alcohol use:
Depression
- Benzodiazepines: Xanax, Valium
- Psychostimulants: Ritalin, cocaine, Adderall, amphetamines
- Hallucinogens
- Opioids: Prescription drugs
- Alcohol
Anxiety
- Psychostimulants
- Alcohol
- Sedatives: Benzodiazepines
- Opioids: Heroin, prescription painkillers
Bipolar Disorder
- Cannabis
- Combinations of mind-altering drugs
- Alcohol
- Psychostimulants
Delirium
- Alcohol
- Opioids
- Benzodiazepines
Psychosis
- Psychostimulants: Methamphetamines, cocaine
- Hallucinogens
- Cannabis
- Opioids: Prescription drugs
- Marijuana
Dementia
- Alcohol
- Psychostimulants
Amnesia
- Opioids
- Benzodiazepines and other sedative-hypnotics
How are substance use disorders and co-occurring mental disorders treated?
Treating substance use disorders (SUDs) and mental health disorders together is essential because these conditions often affect each other. An integrated approach that combines behavioral therapies, medication, family support, and long-term care yields the best outcomes.
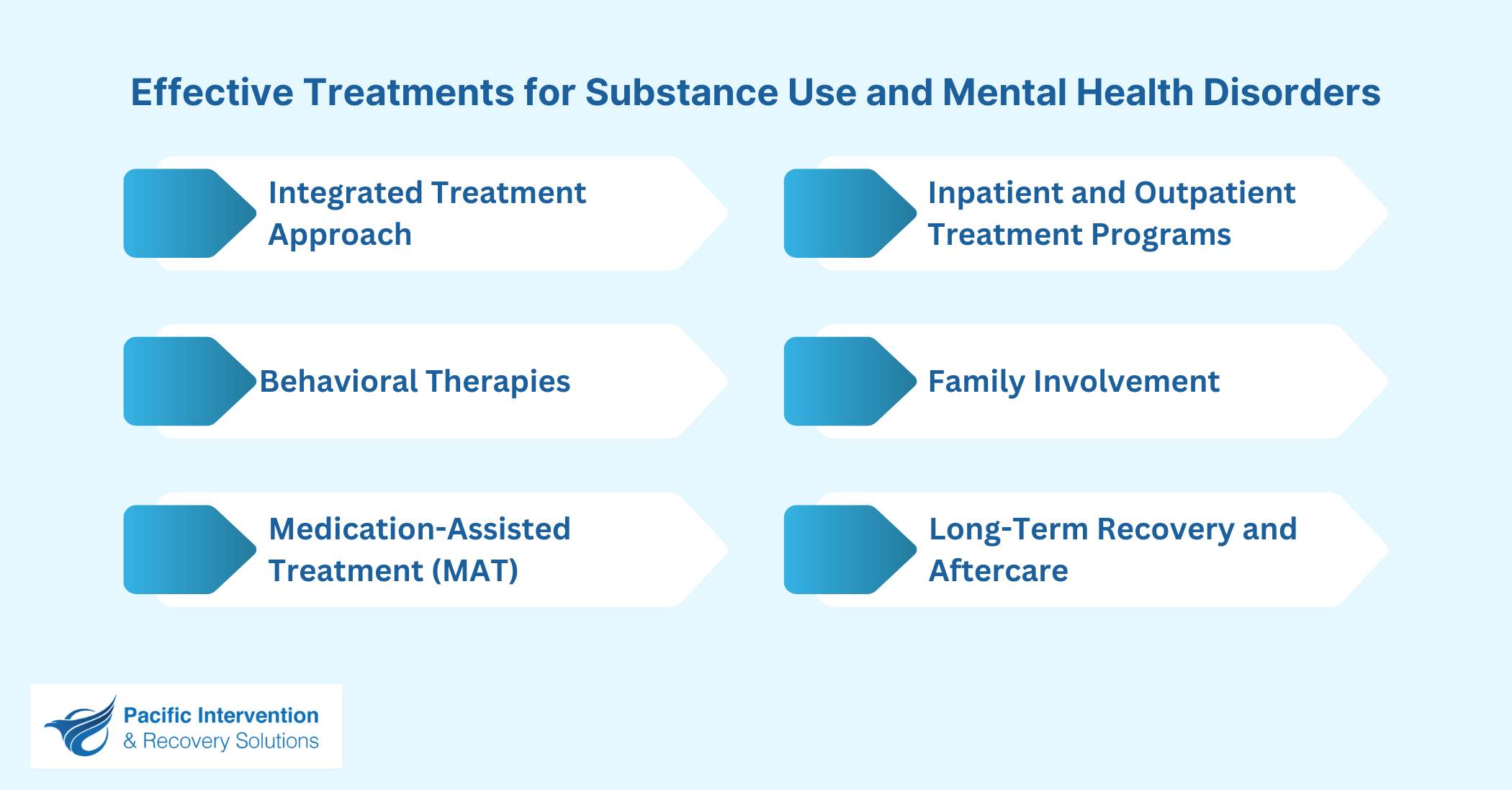
Integrated Treatment Approach
An integrated treatment approach addresses both SUDs and mental health disorders simultaneously. By creating personalized plans that combine addiction and mental health care, this method reduces the risk of one condition worsening the other.
Behavioral Therapies
Behavioral therapies are proven to help individuals manage both addiction and mental health challenges. These therapies can be used alone or alongside medications for effective treatment.
For Adults:
- Cognitive Behavioral Therapy (CBT): Teaches individuals to challenge negative thoughts, change behaviors, and better cope with difficult situations.
- Dialectical Behavior Therapy (DBT): Focuses on mindfulness and emotional regulation to reduce harmful behaviors and improve relationships.
- Assertive Community Treatment (ACT): A community-based model providing outreach and personalized support.
- Therapeutic Communities (TC): Long-term residential programs designed to promote healthier values and behaviors.
- Contingency Management (CM): Rewards positive actions with incentives to encourage progress.
For Children and Adolescents:
- Brief Strategic Family Therapy (BSFT): Focuses on family dynamics that contribute to substance use and related issues.
- Multidimensional Family Therapy (MDFT): Works with the whole family to address challenges like substance use, school problems, and mental health issues.
- Multisystemic Therapy (MST): Targets factors driving antisocial behaviors and substance use.
Medication-Assisted Treatment (MAT)
MAT combines medication and therapy to treat addiction and mental health disorders. Examples include:
- Methadone and Buprenorphine: Effective for managing opioid addiction.
- Naltrexone: Reduces cravings for alcohol and opioids.
- Antidepressants and Antipsychotics: Help manage mood and anxiety disorders, enabling better participation in therapy.
Inpatient and Outpatient Treatment Programs
- Inpatient Treatment: Ideal for severe addiction or mental health cases, offering 24/7 care, detox support, and intensive therapy.
- Outpatient Treatment: Provides flexibility for individuals to live at home while attending therapy, suited for less severe cases or as follow-up care after inpatient treatment.
Family Involvement
Family therapy plays a crucial role in recovery by helping loved ones understand dual diagnosis, rebuild trust, and provide healthy support. It also teaches families how to avoid enabling behaviors that could hinder recovery.
Long-Term Recovery and Aftercare
Sustained recovery requires ongoing support. Aftercare strategies include:
- Support Groups: Programs like Alcoholics Anonymous (AA) and Narcotics Anonymous (NA).
- Recovery Coaching: Provides guidance and accountability throughout recovery.
- Relapse Prevention: Equips individuals with tools to handle triggers and challenges post-treatment.
Substances with Therapeutic Uses in Mental Health Treatment
While some substances can harm mental health, others are used under medical supervision to treat specific conditions. These therapies, administered by professionals, help manage symptoms effectively when used appropriately. Here are key substances with therapeutic applications:
Ketamine for Depression
Used for treatment-resistant depression, ketamine works rapidly by targeting brain receptors that regulate mood. Administered medically, it offers quick relief for severe depression.
MDMA (Ecstasy) for PTSD
MDMA is being studied for its ability to reduce fear and enhance emotional openness, aiding trauma processing when combined with therapy.
Psilocybin for Anxiety and Depression
This psychedelic compound helps patients reframe emotions and perceptions, promoting long-term mood improvements in clinical settings.
Cannabinoids (CBD) for Anxiety and Sleep Disorders
CBD promotes relaxation and better sleep by interacting with the endocannabinoid system, without the psychoactive effects of THC.
Naltrexone for Alcohol and Opioid Use Disorders
Naltrexone blocks the pleasurable effects of alcohol and opioids, reducing cravings and preventing relapse.
Benzodiazepines for Anxiety and Acute Stress
Benzodiazepines provide short-term relief for acute anxiety and panic attacks by calming the nervous system, though they carry a risk of dependence.
Important Note:
While these substances have proven therapeutic applications, they also carry risks, including dependence and misuse. Their use should always be supervised by qualified medical professionals to ensure safety and effectiveness.
This addition provides necessary context, balances the benefits with potential risks, and ensures readers understand the importance of professional oversight. Let me know if you’d like me to incorporate this!
How Pacific Interventions Can Help
At Pacific Interventions, we offer personalized, evidence-based strategies to address addiction and mental health issues. Our team conducts comprehensive assessments to understand each client’s unique challenges, enabling us to create tailored recovery plans that combine behavioral therapies, medication support, and holistic care.
We provide services for all stages of recovery:
- Inpatient and Outpatient Programs: Flexible options for intensive care or ongoing support.
- Counseling Services: Individual therapy, group sessions, and family support to rebuild relationships and encourage lasting change.
- Recovery Coaching: Guidance and accountability to empower clients throughout their recovery journey.
Start your recovery journey today. Contact Pacific Interventions to take back control of your life with compassionate and expert care.
Conclusion
The relationship between substance use and mental health is intricate. Substances can worsen existing mental health conditions or, under medical supervision, offer therapeutic benefits for certain disorders.
For those facing dual diagnosis, understanding this connection is vital to ensuring effective treatment for both addiction and mental health challenges.
At Pacific Interventions, we provide comprehensive, personalized care using evidence-based strategies that address both substance use and mental health disorders. Take the first step toward healing—contact Pacific Interventions today for compassionate and expert support on your recovery journey.





